Overview
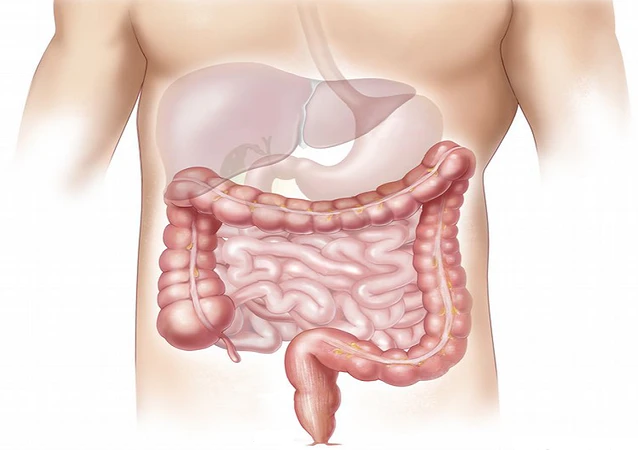
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the large intestine (colon) and rectum. UC causes inflammation and ulcers in the lining of the colon, leading to a variety of symptoms that can significantly impact an individual’s quality of life.
Symptoms
- Diarrhea: This is one of the most common symptoms of UC. It can be watery or bloody and may occur several times a day. Diarrhea can lead to dehydration, electrolyte imbalances, and other complications if not treated promptly.
- Abdominal pain and cramping: UC can cause inflammation and irritation in the colon, which can lead to pain and discomfort in the abdomen. The pain may be mild or severe and can be relieved by passing stools.
- Rectal bleeding: Inflammation in the rectum can cause bleeding during bowel movements, which may appear as bright red blood in the stool or on toilet paper. This can be a scary symptom for many people, but it is a common symptom of UC.
- Urgency: Many people with UC experience a sudden and urgent need to have a bowel movement, which can be difficult to control. This can be particularly distressing when in public or when there are no nearby restrooms available.
- Fatigue: Chronic inflammation can cause fatigue and weakness in people with UC, which can interfere with daily activities and affect the quality of life.
- Weight loss: In severe cases, UC can cause weight loss due to loss of appetite, diarrhea, and malabsorption of nutrients.
- Joint pain: Some people with UC may experience joint pain and swelling, which is a symptom of inflammation in the joints.
- Skin and eye problems: UC can cause inflammation in other parts of the body, such as the skin and eyes. This can cause symptoms such as rashes, redness, and eye irritation.
Causes
- Genetics: UC tends to run in families, and research suggests that genetics play a role in its development. People with a family history of UC are at higher risk of developing the disease themselves.
- Immune system dysfunction: UC is believed to be an autoimmune disease, which means that the immune system mistakenly attacks healthy cells in the colon and rectum, leading to inflammation and damage.
- Environmental factors: Environmental factors, such as exposure to certain bacteria, viruses, or other pathogens, may trigger or exacerbate UC in people who are genetically susceptible to the disease.
- Smoking: Smoking has been shown to increase the risk of UC, and can worsen symptoms in people who already have the disease.
- Diet: While diet does not cause UC, certain foods or dietary factors may trigger symptoms or worsen inflammation in some people. Examples of potential triggers include spicy or high-fat foods, caffeine, alcohol, and dairy products.
- Stress: Stress and anxiety can worsen symptoms of UC, but it is not clear whether stress is a direct cause of the disease.
- Other medical conditions: Certain medical conditions, such as primary sclerosing cholangitis (PSC), can increase the risk of developing UC and makes living with ulcerative colitis all the more challenging.
Diagnosis
Diagnosing ulcerative colitis (UC) can be challenging, as there is no single test that can definitively confirm the disease. Instead, a combination of medical history, physical examination, laboratory tests, and imaging studies may be used to diagnose UC. Here are some common diagnostic tools used in the diagnosis of UC:
- Medical history: Your healthcare provider will ask you about your symptoms, medical history, and family history of digestive or autoimmune diseases. This information can help guide further testing and diagnosis.
- Physical examination: A physical examination may be done to check for signs of inflammation, such as abdominal tenderness, rectal bleeding, or joint pain.
- Blood tests: Blood tests may be done to check for signs of inflammation, such as elevated levels of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). Blood tests can also help rule out other conditions with similar symptoms.
- Stool tests: Stool tests may be done to check for signs of infection or inflammation in the digestive tract.
- Colonoscopy: A colonoscopy is a procedure that allows your healthcare provider to examine the inside of your colon and rectum with a flexible tube with a camera on the end. During the procedure, your healthcare provider may take biopsies (small samples of tissue) to examine under a microscope for signs of inflammation or damage.
- Imaging studies: Imaging studies, such as X-rays, CT scans, or MRI scans, may be done to check for inflammation, swelling, or other abnormalities in the digestive tract.
- Other tests: In some cases, other tests may be done to rule out other conditions or to evaluate the severity of UC, such as an upper endoscopy or a capsule endoscopy
Types
There are two main types of ulcerative colitis (UC), based on the location and extent of inflammation in the digestive tract:
- Ulcerative proctitis: This type of UC affects the rectum and typically extends no more than 15 centimeters into the colon. Symptoms may include rectal bleeding, diarrhea, and an urgent need to have a bowel movement.
- Extensive colitis: This type of UC affects the entire colon, from the rectum to the cecum (the beginning of the colon). Symptoms may include diarrhea, abdominal pain, cramping, fatigue, weight loss, and anemia.
There are also several subtypes of UC, which are classified based on the pattern of inflammation in the digestive tract: - Left-sided colitis: This subtype of UC affects the left side of the colon, from the rectum to the splenic flexure (the bend in the colon near the spleen). Symptoms may include abdominal pain, diarrhea, and rectal bleeding.
- Pan-ulcerative colitis: This subtype of UC affects the entire colon, from the rectum to the cecum. Symptoms may include severe diarrhea, abdominal pain, and rectal bleeding.
- Acute severe colitis: This is a severe and potentially life-threatening subtype of UC that can occur suddenly and require hospitalization. Symptoms may include severe abdominal pain, high fever, rapid heart rate, and dehydration.
Treatment
- Medications: Medications are typically the first line of ulcerative colitis treatment. Anti-inflammatory drugs such as aminosalicylates (e.g. mesalamine, sulfasalazine), corticosteroids, and immunomodulators (e.g. azathioprine, 6-mercaptopurine) can help reduce inflammation and improve symptoms. Biologic drugs, such as anti-TNF agents (e.g. infliximab, adalimumab) and integrin inhibitors (e.g. vedolizumab), may also be used in cases of moderate to severe UC. These medications work by targeting specific proteins in the immune system that contribute to inflammation.
- Lifestyle changes: Certain lifestyle changes can help manage symptoms and make life living with ulcerative colitis easier, including following a low-fiber or low-residue diet, avoiding trigger foods, staying hydrated, getting regular exercise, and managing stress.
- Surgery: In cases of severe UC that do not respond to medication, surgery may be necessary to remove the affected portion of the colon. Surgery can provide a cure for UC, but it does come with risks and may require a permanent colostomy (a surgical opening in the abdomen through which waste is eliminated).
- Alternative therapies: Some people with UC may try alternative therapies, such as probiotics, herbal remedies, or acupuncture. However, the effectiveness of these treatments is not well-established, and they should be used in conjunction with medical treatment, not as a substitute.
Living with Ulcerative Colitis
- Educate yourself: Learn as much as you can about UC, including its symptoms, causes, and treatments. Understanding the disease can help you feel more in control and better able to manage your symptoms.
- Follow your treatment plan: Stick to your treatment plan as prescribed by your healthcare provider, including taking medications as directed and attending regular check-ups. If you’re experiencing side effects or your symptoms aren’t improving, talk to your doctor about adjusting your ulcerative colitis treatment.
- Manage stress: Stress can trigger UC symptoms and makes living with ulcerative colitis even more taxing, so it’s important to find ways to manage stress and anxiety. This could include practicing relaxation techniques such as deep breathing or meditation, getting regular exercise, or participating in activities that you enjoy.
- Keep a symptom diary: Keeping a record of your symptoms can help you identify triggers and patterns, which can be helpful in managing your condition. You can also share this information with your healthcare provider to help guide your treatment.
- Watch your diet: While there’s no one-size-fits-all diet for UC, some people find that certain foods can trigger symptoms. Keeping a food diary and working with a dietitian or nutritionist can help you identify trigger foods and develop a diet that’s right for you.
- Seek emotional support: Living with ulcerative colitis can be emotionally challenging, and it’s important to have a support system in place. This could include talking to family and friends, joining a support group, or seeking counseling.
- Stay active: Regular exercise can help manage stress and improve overall health. Talk to your healthcare provider about the types of exercise that are safe and appropriate for you.
Also read: How To Stop Ulcerative Colitis Flare-Ups
Medical emergency
- Severe abdominal pain: Intense and persistent abdominal pain that is not relieved by over-the-counter pain medications can be a sign of a serious complication, such as a bowel obstruction or perforation.
- Profuse bleeding: If you experience significant rectal bleeding, or if the bleeding is accompanied by other symptoms such as dizziness or fainting, seek medical attention right away.
- High fever: A fever higher than 101°F (38.3°C) can be a sign of a serious infection or inflammation and may require emergency ulcerative colitis treatment.
- Dehydration: UC can cause diarrhea and fluid loss, which can lead to dehydration. Signs of dehydration include dry mouth, dizziness, and decreased urine output. If you’re unable to drink fluids or are experiencing severe dehydration, seek medical attention.
- Rapid weight loss: Unintentional weight loss can be a sign of malnutrition or a more serious complication of UC, such as bowel obstruction or perforation.
- Infection: People with UC are at increased risk of developing infections, particularly if they are taking immunosuppressant medications. If you develop symptoms of an infection, such as fever, chills, or cough, seek medical attention right away.
- Pregnancy: Women living with ulcerative colitis who are pregnant or planning to become pregnant may require specialized care to manage their condition and ensure a healthy pregnancy. It’s important to work closely with your healthcare provider to develop a plan for pregnancy and postpartum care.
Citation
https://en.wikipedia.org/wiki/Ulcerative_colitis
https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/crohns-disease-and-ulcerative-colitis
Featured pic: https://tinyurl.com/pdau3vkt